With Instructor Anthony Von der Muhll, L.Ac., DAOM, DNBAO, FAIPM
Self-Paced Distance Learning
Includes lifetime access to high-definition videos, slideshows, and class notes -- see below for detailed description of contents
Head, Neck, Thorax: History, Examination, Assessment, & Treatment
Comments from Course Evaluations
"This class was amazing and so packed with information. I am going to have to listen to the recording over and over in order to be able write down all that was said. I can't wait to be able to take an in person course." -- Shelby Smith, L.Ac., Olympia, Washington
"This class has been incredibly enriching and full of valuable information. I truly enjoyed every session and felt fully engaged throughout. The depth of knowledge shared, especially regarding assessment techniques and the integration of orthopedic tools, has greatly expanded my understanding of clinical applications in acupuncture. I feel more confident in my ability to evaluate and treat complex cases, and I’m excited to apply what I’ve learned in my practice. This has definitely been one of the most informative and inspiring courses I’ve taken!" -- Karla Colmenarz, L.Ac., Chevy Chase, Maryland
Clinical anatomy, kinesiology, and the jing-jin ("sinew meridians" or myofascial tracts)
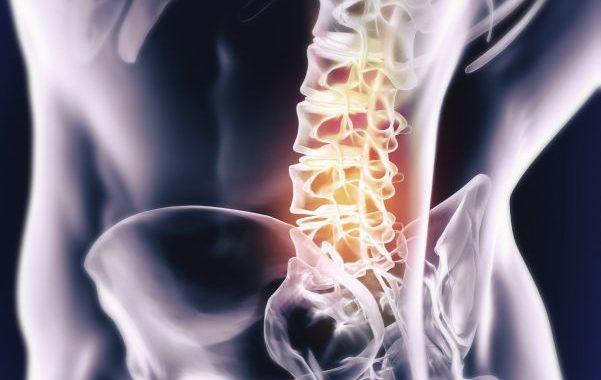
- Bones, muscles, discs and facet joints, and neurology
- Posture and motion dysfunctions
- The arthritic progression: strain/sprain, derangement, degeneration
History-taking for head, neck, thorax: key diagnostic questions
- "Red flag" symptoms of urgent/serious medical conditions warranting referral to physician care
- Differentiating symptoms of muscles, joint, disc, and spinal cord, plexus and nerve root injuries
- Neural hypersensitization and psycho-social factors
- Functional capacity questionnaires for reporting to managed care insurance
Physical exam of the head, neck, thorax: key procedures
- Observation, inspection and palpation
- Joint exam: active range-of-motion, stability, and tracking assessment of the cervical and thoracic spine and TM joint
- Neurologic exam: upper motor neuron; arm reflex, sensory, and motor function; and brachial plexopathies
- Special orthopedic tests for the spine and ribcage
- Documentation of physical exam findings
- Measuring and reporting functional capacity baselines and treatment outcomes
Diagnosis and pattern identification
- Cervicogenic and tension-type headaches
- Temperomandibular joint pain and dysfunction
- Cervical and thoracic sprains/strains and chronic myofascial pain
- Cervical and thoracic disc and facet joint injuries: dysfunction, derangement, degeneration
- Nerve root and spinal cord injuries
- Intercostal sprains/strains
- Brachial plexopathies and thoracic outlet syndrome
- Myofascial trigger points and referred pain patterns for over 17 muscles of the head, face, neck and thorax
Treatment of head, neck, and thorax pain and injuries
- When and how to use distant and local needling for rapid and lasting pain relief
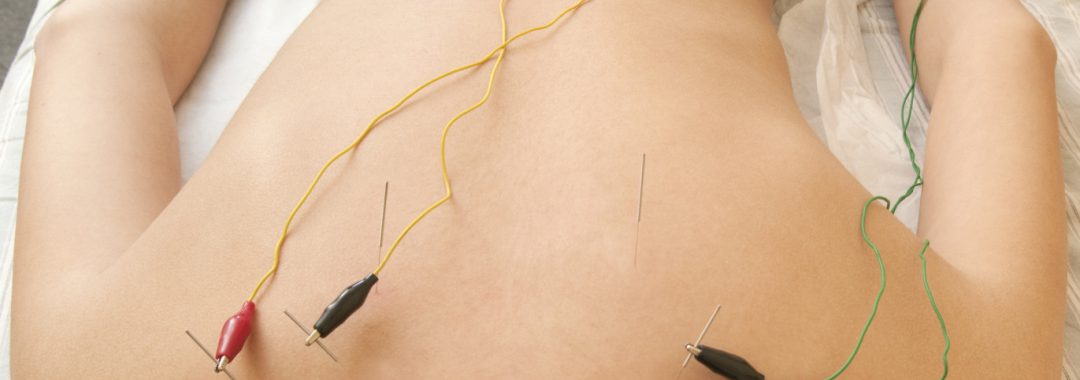
- Electroacupuncture for neural blockade and rehabilitation
- Releasing muscle tension through myofascial trigger point needling
- Prolo-acupuncture for spinal and TM joint stabilization and mobilization
- Using 7-star, 3-edged and lancet needles to reduce inflammation and ischemic pain
- Manual therapy: gua sha, tui na, and muscle energy techniques to reduce trigger points and restore muscle flexibility and joint range of motion
- Active suction cupping: combining cups with passive and active movement for rapid and lasting results
- Postural and ergonomic correction and exercise therapies
Get the most out of your learning experience!
- Prepare for the class with the Anatomy for Acupuncturists Lab
- Then build on and consolidate your skills with the Review/Practicum Lab
Student Ratings and Comments
from evaluations as required by California Acupuncture Board, prior live class offerings in 2017.
Respondents: 20 of 20 enrolled